What is Gastroesophageal reflux disease(GERD) ?
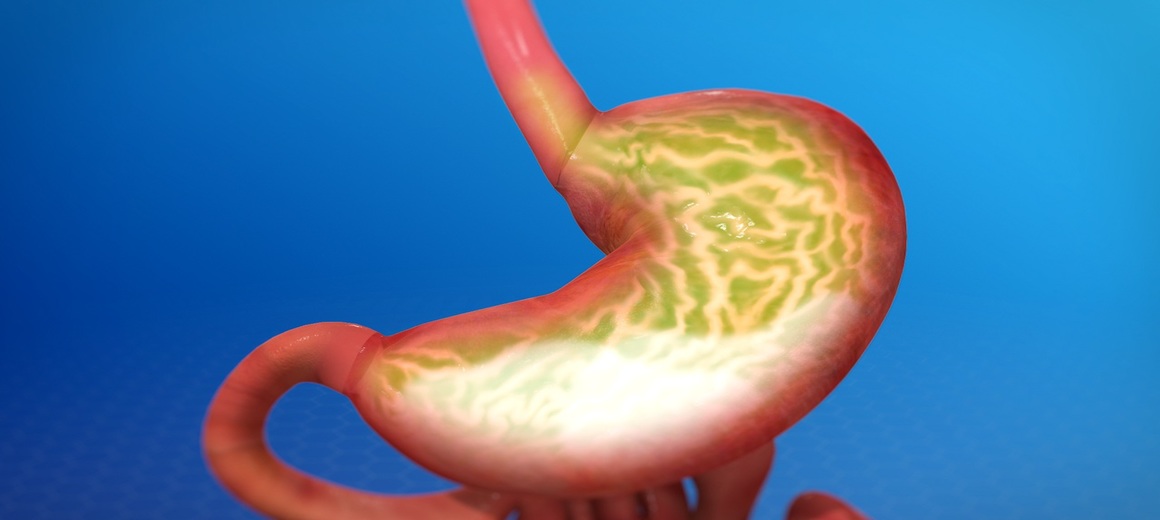
Gastroesophageal reflux is a physical condition in which acid from the stomach flows backward up into the esophagus. People will experience heartburn when excessive amounts of acid from the stomach refluxes into the esophagus.
Many describe heartburn as a feeling of burning discomfort, localized behind the chest, that moves up toward the neck and throat. Some even experience the bitter or sour taste of the acid in the back of the throat. The burning and pressure symptoms of heartburn can last for several hours and often worsen after eating food and even mimics a heart attack.
All of us may have occasional heartburn. However, frequent heartburn (two or more times a week), food sticking, blood in throat or weight loss may be associated with a more severe GERD. Most people will experience heartburn if the lining of the esophagus comes in contact with too much stomach juice for too long a period of time. This stomach juice consists of acid and digestive enzymes. The prolonged contact of acidic stomach juice with the esophageal lining injures the esophagus and produces a burning discomfort.
Normally, a muscular valve at the lower end of the esophagus called the lower esophageal sphincter or “LES” keeps the acid in the stomach and out of the esophagus. In GERD the LES relaxes too frequently, which allows stomach acid to reflux, or flow backward into the esophagus.
GERD can also have extra-esophageal manifestations like chest pain, asthma, chronic cough, ear, nose and throat problems which often avoid detection.
What types of tests are needed to evaluate GERD?
Often GERD can be clinically diagnosed basing on complaints of the patient. Additional tests may be required when it is unclear whether your symptoms are caused by acid reflux, or if you suffer from complications of GERD such as dysphagia (difficulty in swallowing), bleeding, choking, or if your symptoms fail to improve with prescription medications.
In all these conditions additional tests are to be conducted to confirm the diagnosis: Endoscopy, Esophageal Manometry or Esophalgeal pH, Upper GI barium Series.
Lifestyle Changes to Reduce GERD
- Avoid foods and drinks that trigger heartburn.
- Small frequent meals are preferred.
- Do not lie down after you eat for about 3 hrs.
- Stop using tobacco in any form.
- Do not consume excess alcohol.
- Avoid wearing tight clothes across your waist, stomach, or abdomen.
- Loose weight if you are overweight.
- Raise the head of your bed 6 to 8 inches can help in reducing reflux frequency.
- Limit or reduce stress in your life.
- Try participating in an exercise, yoga or meditation program.
- Take your medicines as your doctor prescribes.
Avoid Foods which can increase reflux:
- Coffee, tea, and soft drinks that contain caffeine.
- Citrus juices and drinks, such as orange, grapefruit, lemon, lime, pineapple.
- Fatty or fried foods.
- Peppermint or spearmint, including flavouring.
- Spicy, highly seasoned foods.
- Chocolate and sweets can also increase symptoms.
FAQs:
Should I avoid Tea or coffee completely?
Not really. However excess coffee and tea can be harmful.
Can I take alcohol?
Alcohol in moderation may not harm. However excess alcohol can lead to complications.
How to avoid nocturnal burning?
Early dinner, raising head end and may need additional medication. What can be done if not responding to standard medication? If you are not responding to standard medication the options are to change the drug or to increase dosage which will be decided by your doctor.
When should I require surgery?
In general most of GERD patients respond to standard medication when followed properly. A small number of patients who do not respond to long term medical therapy or have a large hiatus hernia may need surgical correction.
